Medication For Pelvic Floor Spasms

This typically involves a course of treatment with weekly to biweekly office sessions over 8 12 weeks.
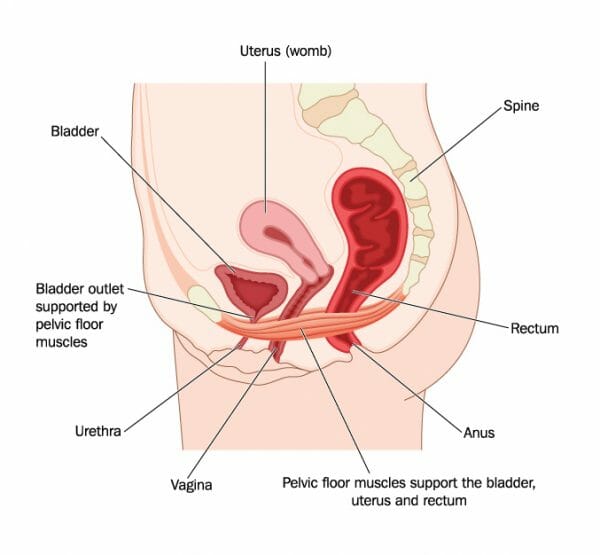
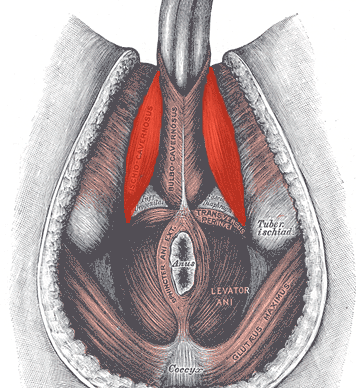
Medication for pelvic floor spasms. Pelvic floor therapy with biofeedback and stimulation collectively referred to here as pft is the chief strategy that works to relieve problems associated with pelvic floor spasm. Your doctor may prescribe a muscle relaxant to help with pelvic floor dysfunction symptoms. The mainstay of treatment for pelvic floor spasm is physical therapy pt that consists of myofascial release posture improvement and muscle stretching exercises. Daily medications that help to keep your bowel movements soft and regular are a very important part of treating pelvic floor dysfunction.
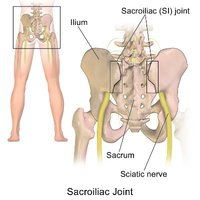
Other treatment options include. Some of the main treatments to relieve pelvic muscle spasms are pelvic floor physical therapy which includes myofascial release improving posture and pelvic floor muscle stretching. Prescription drugs can help relieve the pain and discomfort from muscle spasms or spasticity. Therefore kegel exercises which are often inappropriately applied as generic physical therapy can make the symptoms worse.
The second main treatment for pelvic floor muscle spasm is the use of botulinum toxin a botox. Some of these medications are available over the counter at the drugstore and include stool softeners such as miralax colace senna or generic stool softeners. In addition certain over the counter medications may be used to treat aches and pains associated with. The relaxants can prevent your muscles.
6 the goal is to help relax the muscles not to strengthen them. Treatment with muscle relaxants predominantly diazepam 2 10 mg bid qid can help control acute pain spasm and maintain an adequate level of muscle relaxation in order to proceed with biofeedback or massage. To reduce strain on your pelvic floor muscles avoid pushing or straining when using the bathroom. If pelvic floor spasms are diagnosed treatment is often provided by a physical therapist and may include avoiding activities that aggravate the symptoms such as cycling with a seat that s too hard or doesn t fit ergonomically behavioral changes such as not holding in urine if you have to go and education about the pelvic floor.